Unlike migraines and other headaches that stem from issues in the brain, cervicogenic headaches originate in the cervical spine region — in the bones, discs, or soft tissues of the neck — and can be quite different from a typical headache. Most people who experience migraines or frequent headaches can identify a trigger. With cervicogenic headaches, there are no triggers as they are caused by physical problems. Cervicogenic headaches are not well understood and are therefore difficult to diagnose and treat.
A Secondary Headache
Experts believe cervicogenic headaches are secondary pain, meaning that an issue originating somewhere other than the head causes them. This is commonly called “referred pain.” Though understanding about cervicogenic headaches is limited, it is likely that the pain originates near where the skull meets the top of the neck, the cervical vertebrae. The headache can also include pain generated in the ligaments, joints, nerves, or blood vessels.
More Than a Headache
It is important to remember that a diagnosis of cervicogenic headaches involves much more than the headache itself. Doctors must also identify the issue in the neck that is causing the pain. Some things that can cause cervicogenic headaches are fractures, infections, tumors, and rheumatoid arthritis of the upper cervical spine. Age-related changes to this area, cervical spondylosis, may cause cervicogenic headaches, too.
Diagnostic Criteria
Though difficult to diagnose, but there are a few criteria clearly associated with cervicogenic headaches. People who develop them experience pain that starts on one side of the back of the head and neck and moves to the front and may even extend into the arm. Neck pain and stiffness are also common and can be aggravated by maintaining sustained neck positions common in certain professions, including carpentry and truck driving.
Prevalence
Cervicogenic headaches may be more common than we would assume. An estimated 47% of people in the world experience regular headaches or migraines. Of these, it is believed that as many as 20% are cervicogenic in nature. Women are four times more likely to experience them than men, which may indicate a hormonal factor. Additionally, there may also be a connection to temporomandibular joint (TMJ) issues, as up to 44% of people with cervicogenic headaches have TMJ problems, too.
Symptoms
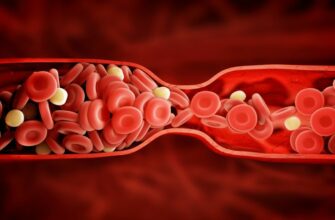
Headache and neck pain are the two biggest signs of cervicogenic headaches, but other specific symptoms can indicate a serious issue. Vertebral artery dissection — a common cause of stroke in children, young adults, and those experiencing physical trauma — can present as head and neck pain. If the pain is accompanied by vision problems or dizziness, gets worse over time or comes on suddenly, or occurs following a head or neck injury, the person should go to the emergency room.
Possible Classifications
Cervicogenic headaches are secondary pain, and identifying the root cause is essential. There is some thought that researchers should further classify cervicogenic headaches into those caused by trauma and those resulting from other factors. One reason is that musculoskeletal assessment is key to diagnosis, and people experiencing neck trauma may have different symptoms than those whose headaches have other causes.
Assessment
Assessment of a cervicogenic headache is quite involved. Forward head posture is common, which may indicate weak muscle tone, specifically in the deep neck flexors, though this requires more research. Muscle tightness is often present across the neck, chest, and shoulders. Electromyography (EMG) shows high responsiveness in the sternocleidomastoid muscle, the largest muscle in the neck, responsible for flexion and rotation to the opposite side, and a decreased response from the deep neck flexors.
Additional Findings
Assessment of cervicogenic headache may also include palpable joint dysfunction, pain with passive movement, and restricted range of motion. Soft tissue assessment could show trigger point pain on the symptomatic side which, when palpated, reproduces headache pain in 50% of cases. Some people with cervicogenic headaches may also demonstrate abnormal breathing patterns due to muscle tightness affecting the accessory breathing muscles. Note that there is not complete agreement about the findings of these assessments, as more research is needed.
Treatment Approach
The first line of treatment for cervicogenic headaches is medication, but it is minimally successful as it does not fix the cause of the pain. Some people with cervicogenic headaches do not respond to this treatment and may require nerve blocks and steroids. Accurate diagnosis is essential for treatment to be successful, and physicians should also consider concurrent conditions like TMJ disorder.
Modalities
Sports physical therapists use various treatment modalities, but there are few studies on their efficacy. Most studies focus on manual therapy, specifically joint mobilization and manipulation and spinal manipulative therapy focused on the upper cervical spine. While trials suggest that manual therapy results in better outcomes, high-quality studies are still needed. Muscle stretching may also reduce muscle tightness across the neck, chest, and shoulders and may relieve trigger pain.

 Home
Home Health
Health Diet & Nutrition
Diet & Nutrition Living Well
Living Well More
More