As the global prevalence of chronic diseases rises, the rates of skin ulcers, and all the complications that accompany them, increase with it. As the population ages, wound care becomes a more vital practice. The good news is that advancing technologies ensure treatments are keeping pace with need.
Skin Ulcer Stages
There are four stages of skin ulcer development. At stage 1, texture and color change, swelling occurs, and the area feels warmer than normal. The top layer wears away in stage 2, forming a tender, painful sore. At stage 3, the tissue beneath the skin further erodes, resulting in a small crater and, in some cases, visible fatty tissue. The final stage involves necrosis, which can inflict extensive damage to muscles, bones, and tendons.
Stasis Dermatitis
Individuals over 50, particularly women with poor circulation, are at risk of stasis or gravitational dermatitis. This type of skin inflammation happens in the lower legs, usually close to the ankles. The resulting swelling puts pressure on the skin’s blood vessels. In the earlier stages, people experience a noticeable itch. Scratching leads to cracking, ulcers, and scars.
Pressure Ulcers
Pressure ulcers, also known as bedsores, are a significant risk for people who are bedridden or in a wheelchair. The sustained pressure, friction, or shear on certain points of the body causes compressed or distorted vessels, which impede blood flow. Without the proper nutrients coming into the area or a way to remove localized metabolic waste, painful swelling develops, and open wounds may result if the issue is left untreated.
Neuropathic Ulcers
Neuropathic ulcers are a potential complication in people with diabetes. Those with uncontrolled or poorly controlled high blood sugar may experience tingling or stabbing pains in their extremities. Chronic hyperglycemia damages the nerves, resulting in poor or no sensation, particularly in the feet. This means that minor cuts go unnoticed and untreated, leading to the breakdown of the tissue, and eventually ulcers.
Leg Ulcers
Arterial and venous ulcers usually affect the legs. Arterial ulcers are caused by reduced arterial blood supply due to atherosclerosis, persistent hypertension, or other vascular diseases. They produce lesions in the tunica intima, the innermost layer of the artery, and diminished blood supply causes skin layer damage. With venous ulcers, the valves in the veins that prevent blood flow reflux malfunction, leading to fat layer inflammation.
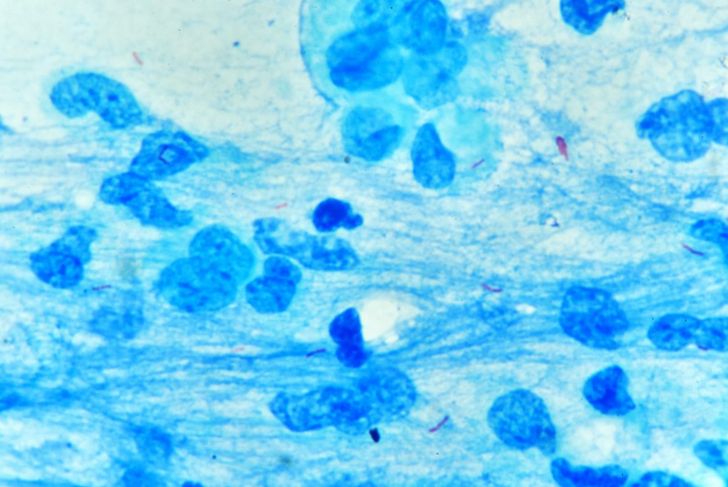
Buruli Ulcer
Buruli ulcer is a disease that is caused by Mycobacterium ulcerans, a bacteria in the same family as leprosy and tuberculosis, found in tropical areas of West Africa and Australia. This bacterium produces a toxin called mycolactone, which is primarily responsible for the extensive tissue damage associated with this condition. Skin ulcers, infection, and damage can extend all the way down to the bone.
Treatments Available
Proper treatment of ulcers depends on timing, location, and the stage. Doctors must first reduce the risk of infection, which requires antibiotics. Stemming blood clotting while applying topical treatments and dressings is also essential, especially for people with ulcers on their feet. In many cases, advanced tissue damage requires removal or debriding.
Osteomyelitis
Osteomyelitis is inflammation of the bone and marrow and is most commonly found in the femur and tibia. People with pressure ulcers and foot injuries due to diabetic neuropathy are more likely to experience this complication. Osteomyelitis is the result of diminished blood flow to certain areas, like the hips, lower back, and legs.
Sepsis
People with skin ulcers around the genitals, buttocks, or tailbone tend to have increased risk of developing sepsis, because feces and urine may come in contact with the wounds. Infected wounds can lead to sepsis. If they are wearing adult diapers, that enclosed, warm, humid environment allows pathogenic germ colonization, especially at more advanced stages of skin damage.
Remedies and Prevention
Because preexisting conditions, such as diabetes, increase the risk of ulcers, people with these diseases should examine the skin of their legs and soles of the feet regularly and ensure their toenails are always smoothly trimmed, to prevent injury. For preventing ulcers related to poor circulation, doctors recommend wearing compression socks and keeping legs elevated. If a sore is discovered, the best way to prevent it from worsening is to wash it with a mild soap daily, dry well, and carefully apply a dressing.

 Home
Home Health
Health Diet & Nutrition
Diet & Nutrition Living Well
Living Well More
More