Parasomnias are sleeping disorders that occur during REM sleep and affect one’s ability to achieve proper rest. Sleep paralysis is one of the more frightening parasomnias because it renders the individual unable to move for short periods of time. Approximately 30 percent of people experience a sleep paralysis event at least once in their life. For some, however, it is a chronic condition that persists for years and can cause and is caused by various issues.
Triggers
One of the major causes of sleep paralysis is lack of sleep, which affects between 35 and 40 percent of adults. Changing work schedules, jet lag, and stress also contribute to sleep deprivation. Most people experience their first incident of sleep paralysis in adolescence, and they become more frequent in adulthood. Sleep deprivation fragments the rapid eye movement cycle when the body is naturally paralyzed during dream states. When the body is out of sync with the brain, the latter can achieve a level of consciousness, while the body remains paralyzed.
Hallucinations
Art history is full of works depicting someone sleeping with a demon on their chest or a dark, menacing figure hovering above. While dramatic, some experts believe these terrifying visualizations could, in part, be a result of a sleep paralysis episode. Researchers have found that during sleep paralysis, select serotonin receptors are activated, causing vivid, frightening hallucinations.
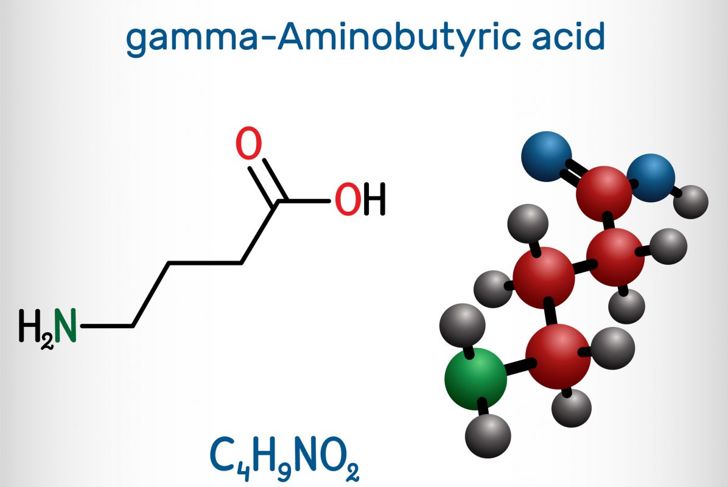
GABA and Glycine
GABA or gamma-aminobutyric acid is a calming neurotransmitter that helps ease stress and may also prevent seizures. It enables the body and mind to relax and sleep soundly. Glycine is another amino acid and neurotransmitter that increases serotonin levels and improves sleep quality. Initially, doctors assumed that glycine was the culprit, but later studies found that blocking both GABA and glycine neuroreceptors resulted in sleep paralysis.
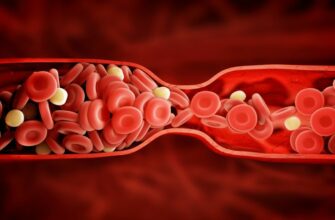
Connection to Hypertension and Panic Disorder
Isolated sleep paralysis, ISP, is when the condition occurs absent of any other type of parasomnia. In a study of 31 African American men and women, close to 42 percent had episodes of ISP. Researchers believe that excess stress leads to panic manifestations that cause episodic hypertension, and the response to adrenergic stimuli results in bouts of isolated sleep paralysis. Doctors also believe that there could be some adrenergic dysfunction specific to hypertension that causes both ISP and panic disorder symptoms.
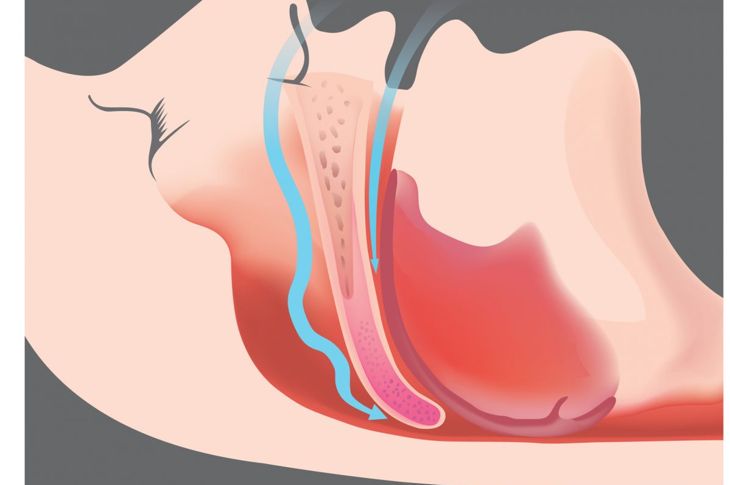
Obstructive Sleep Apnea
Obstructive sleep apnea is more dangerous than regular sleep apnea because the stop and start phenomenon is caused by the intermittent relaxation of the throat muscles, which blocks the airway. Usually, heavy snoring is a key indicator of this condition, but a nine-year study showed that bouts of isolated sleep paralysis may also be a symptom of this type of apnea.
MDMA
Methylenedioxymethamphetamine or MDMA, sold as the recreational drug ecstasy, is a toxin. While it provides a feel-good effect at first, when the drug metabolizes, it creates by-products in the brain that lead to shortened, disturbed sleep cycles and altered serotonin neurotransmission, resulting in sleep paralysis. While no clinical studies link ecstasy to sleep paralysis, anonymous reports from past and present users state that not only did they experience sleep paralysis, but it was prolonged, with more vivid, nightmarish hallucinations.
Sleep Paralysis and Narcolepsy
Statistics show that between 20 and 50 percent of people with narcolepsy experience sleep paralysis, specifically hypnagogic sleep paralysis. Essentially, the muscle paralysis that typically occurs during REM sleep happens when they suddenly fall asleep. Because the natural line between sleep and wakefulness is blurred, those with narcolepsy may even experience muscle paralysis while they are awake.
Sleep Paralysis and Neurodegeneration
Muscle paralysis during REM sleep is a normal safety mechanism. If this paralytic process is impaired, people may physically act out their dreams, in some cases injuring themselves and their partners. Researchers have found that this type of REM sleep behavior disorder can precede neurodegenerative diseases, such as Parkinson’s and Alzheimer’s. The cumulative sleep deprivation contributes to cognitive dysfunction related to neurodegeneration, and once neurodegeneration starts, it worsens sleep deprivation, creating a cruel cycle.
Diagnosis and Treatment
Isolated sleep paralysis is common and may not affect general health. Recurrent sleep paralysis that causes daytime sleepiness requires an overnight sleep study. This involves charting vital statistics, such as breathing, heartbeat, and muscle movements with the help of tools like polysomnograms and electromyograms. Taking care of the underlying issues — psychiatric or stress triggers, for example — usually resolves the disorder. In some cases, doctors prescribe antidepressants, as they tend to help with the chemical aspects of the condition.
Breaking Free
Episodes of sleep paralysis are short but can seem far longer. Waking up from sleep paralysis takes concerted effort, according to those who experience it. To break free, some recommend wiggling the toes, while others suggest asking a partner to wake you if your breathing is uncharacteristically ragged and uneven. Remembering that sleep paralysis is not inherently life-threatening can help you navigate through the episodes.

 Home
Home Health
Health Diet & Nutrition
Diet & Nutrition Living Well
Living Well More
More