Antiphospholipid antibody syndrome (APS) is a rare autoimmune disorder that causes the immune system to create antibodies that attack cells and tissues. The condition is also known as anticardiolipin antibody syndrome, antiphospholipid syndrome, Hughes syndrome, Lupus anticoagulant syndrome, aCL syndrome, and aPL syndrome. The disease is noticeably more prominent in young women than in any other demographic, and it carries significant health risks. APS also tends to occur alongside other diseases and disorders.
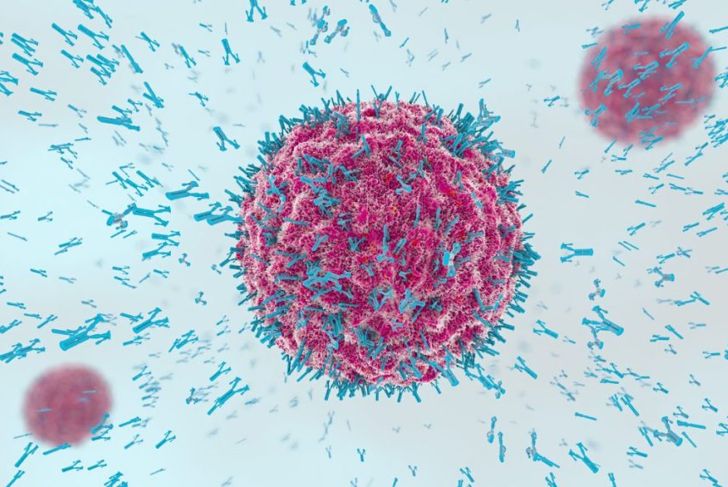
What are Antibodies and Phospholipids?
Antibodies are a special type of protein. Usually, their purpose is to help fight infections and defend the body. Antiphospholipid antibody syndrome creates antibodies that target natural phospholipids rather than dangerous materials. Phospholipids are fats that exist in all living cells and cell membranes. They perform many important functions depending on the cell and are necessary for life. Antiphospholipid antibodies attack phospholipids and damage the cells, causing a range of issues.
Cause
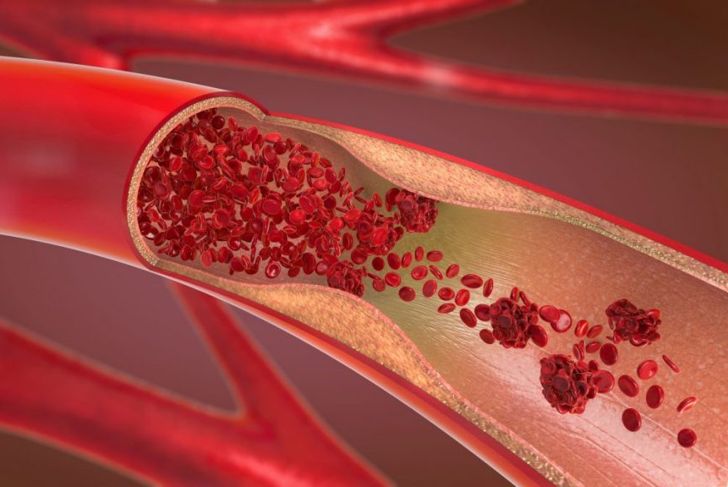
Researchers still lack information about antiphospholipid antibody syndrome and its various effects. Most of the symptoms develop because the destruction of phospholipids leads to the formation of blood clots. However, researchers don’t know why the blood clots form or what causes the immune system to create antiphospholipid antibodies in the first place. Most doctors believe that the disease is the result of external influences and other conditions. In terms of blood clots, some experts believe that the antibodies damage the inner lining of the blood vessels, thus forming blood clots. Others think that the blood clots are already present and damaging the blood vessels, so the body creates antibodies to destroy them.
Common Symptoms
Symptoms of antiphospholipid antibody syndrome are dependent on the size and location of blood clots. Some of the more major signs and symptoms are:
Warmth, redness, pain, and swelling in the limbs
Chronic and persistent headaches
Upper body and head discomfort
Chest pain and breathing issues
Nausea
Speech issues
Some people with the syndrome develop thrombocytopenia, which means that the blood has a low number of platelets. In some instances, the individual may have internal bleeding.
Effects on Pregnant Women
In addition to the common symptoms of antiphospholipid antibody syndrome, other factors can cause more specific issues. Young pregnant women are particularly prone to developing the condition. Preeclampsia is high blood pressure that occurs during pregnancy. Though it is common for pregnant women to have higher blood pressure, antiphospholipid antibody syndrome can cause preeclampsia to progress to eclampsia, which can lead to seizures.
Possible Complications
Antiphospholipid antibody syndrome can lead to life-threatening complications such as heart attacks, strokes, and kidney damage. If a blood clot forms in a deep vein in the leg, thigh, or pelvis, it may cause deep vein thrombosis or DVT, which causes shortness of breath and chest pain and can be fatal. Pulmonary embolisms are also common. Pregnant women have a higher risk of stillbirths and miscarriages, though many women with the syndrome have healthy and successful births with proper medical care.
Risk Factors
Antiphospholipid antibody syndrome affects five times more women than men. Most people develop the condition between the ages of 30 and 40. Additionally, people with other autoimmune conditions are more likely to develop antiphospholipid antibody syndrome. Individuals with syphilis, hepatitis C, Lyme disease, or HIV/AIDS are also at a greater risk. Researchers have also linked some blood pressure medications to the syndrome. APS can also run in families.
Diagnosis
Doctors are usually able to diagnose antiphospholipid antibody syndrome by looking at their patient’s family history and performing diagnostic tests. In some cases, physicians take blood tests that show the presence of antiphospholipid antibodies, but the patient does not have any other symptoms. The presence of the antibodies alone is not enough to diagnose APS. There must be a history of health problems that result from the disorder for diagnosis, otherwise, the antibodies are a unique trait and not a disease.
Treatment
There is currently no cure for antiphospholipid antibody syndrome, but medications can help prevent complications. The most common medications for treating this syndrome are anticoagulants, also known as blood thinners. These anticoagulants help break up blood clots and prevent them from growing. Doctors can administer anticoagulants in pill or IV form, and may use a combination of both. Physicians may also need to balance treatment for other existing conditions, as well. In most cases, combating the symptoms of a coexisting condition helps with APS symptoms.
Treatment During Pregnancy
A pregnant woman can have a healthy and successful pregnancy even if she has antiphospholipid antibody syndrome. However, pregnant women require more care and specific medications. Some anticoagulants can harm the fetus, so doctors need to be knowledgeable on the best approach. In some cases, the expectant mother requires a blood or disease specialist who is familiar with APS. Children of mothers with the syndrome often have slower development in the womb, which may require medical evaluation.
Living with APS
Despite the condition having no cure, it is possible to control antiphospholipid antibody syndrome and live a normal life. Individuals with the condition should follow their doctor’s orders closely and remain in regular contact. It is important to let the physician know of any changes in symptoms, diet, or lifestyle. Regular medical checks are also necessary, particularly for women who might become pregnant. In some cases, an individual may need to make dietary changes, as some foods interact poorly with anticoagulants.

 Home
Home Health
Health Diet & Nutrition
Diet & Nutrition Living Well
Living Well More
More