Gastritis, sometimes called dyspepsia, is inflammation of the lining of the stomach. Reddening and swelling of the stomach lining can occur quickly — an acute case — or develop gradually in chronic cases. Pangastritis is gastritis that affects the entire stomach. Erosive pangastritis causes shallow sores, known as erosion, on the stomach lining. Eight out of every 1,000 people will experience acute gastritis at some point, while two out of every 10,000 people develop chronic gastritis.
Symptoms of Pangastritis
A throbbing, dull, or burning pain in the upper part of the stomach is a common system of pangastritis. Other symptoms include loss of appetite, nausea, vomiting, heartburn, frequent burping, hiccups, and abdominal bloating. Chronic pangastritis may lead to unintentional weight loss and fatigue. In rare cases, gastric polyps and malignant or benign tumors occur as a result of chronic pangastritis.
Causes of Pangastritis
Long-term use of nonsteroidal anti-inflammatory drugs, NSAIDs, is a common cause of pangastritis. Other risk factors include tobacco products, alcohol, some recreational drugs, large doses of vitamin or mineral supplements, chronic stress, frequent vomiting, radiation during cancer treatment, and bacterial infection from H. pylori. Stress gastritis or pangastritis can be a result of injuries, illness, burns, or surgery.
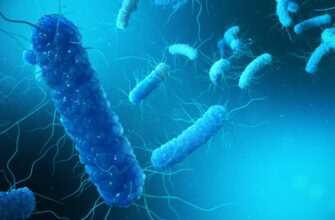
H. pylori
Helicobacter pylori or H. pylori is a bacteria found inside the stomach. H. pylori is very common and some researchers estimate that over half of the population in the entire world carries the bacteria. Most people never experience negative effects, but an infection of H. pylori increases the risk of developing stomach cancer, gastritis, and peptic ulcers.
Pangastritis and Chronic Disorders
Pangastritis can be a result of other diseases or disorders. Bile reflux causes bile, a liquid secreted by the liver to aid in digestion, to back up into the stomach. Crohn’s disease, ulcerative colitis, and Celiac disease may present with pangastritis. Autoimmune disorders cause pangastritis when immune cells attack healthy tissue in the stomach.
Complications
People with pangastritis should seek emergency care if chest pain starts suddenly, worsens, or spreads to the back, neck, shoulders, or arms. Intense stomach pain that moves to the lower-right area of the abdomen and frequent vomiting are emergencies as well. Other symptoms that require immediate medical attention are difficulty breathing or swallowing, confusion, rapid heartbeat, extreme drowsiness or difficulty waking up, fainting, and blood in vomit or stool. Blood in stool looks black and tarry, while blood in vomit looks like coffee grounds.
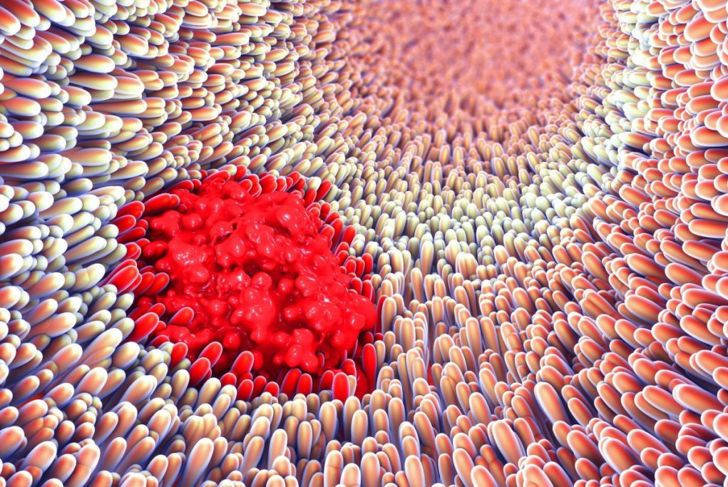
Disease Process
The internal lining of the stomach is a mucous membrane called the gastric mucosa. Three glands in the gastric mucosa produce stomach acid and an enzyme known as pepsin. Stomach acid breaks down food and pepsin digests protein. The stomach lining is coated with a thick mucus layer to protect it from digestive acids. If the mucus becomes too thin, the acids damage the stomach lining.
Easing Pangastritis with Diet
Proper diet and nutrition can relieve symptoms of pangastritis. People with the condition should limit fats since high-fat diets have been shown to increase stomach inflammation. Broccoli contains a nutrient called sulforaphane that may inhibit the growth of H. pylori. Some doctors recommend probiotics. If supplements irritate the stomach lining, foods like yogurt, sauerkraut, and sourdough bread also contain probiotics. A high-fiber diet is good for the entire digestive system and absorbs some excess stomach acid. Apples, celery, berries, olive oil, honey, and herbal teas may help relieve heartburn and discomfort. Small meals five or six times throughout the day are easier to digest than two or three large meals.
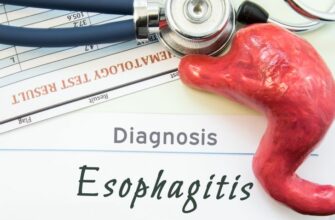
Diagnosis
Medical history and reported symptoms are the most common methods by which doctors diagnose gastritis. A biopsy during an upper endoscopy can indicate the presence of pangastritis. The pathologist looks for a red lining and inflammation. Lab analysis can identify white blood cells, mostly leukocytes. Active bleeding in some areas, and pitted sores, can indicate erosive gastritis.
Treatment
Doctors usually prescribe medications to treat pangastritis. H. pylori infections receive antibiotics for approximately two weeks. Antacids to neutralize stomach acids, along with anti-nausea medications, relieve discomfort. Proton pump inhibitors and H2 blockers lessen the amount of stomach acid the body produces. Surgery is only for severe cases when erosive sores or ulcers wear through the stomach.
Outlook
The gastric mucosa rarely returns to a completely normal and healthy state after chronic pangastritis. Severe changes in the mucosa or the presence of pre-cancerous lesions may require monitoring with an annual upper endoscopy. Pernicious anemia from pangastritis is not always reversible. It develops due to a lack of a specific substance in the stomach necessary for digestion and absorption of vitamin B12. If pernicious anemia persists after treatment for pangastritis, regular B12 injections can help manage symptoms.

 Home
Home Health
Health Diet & Nutrition
Diet & Nutrition Living Well
Living Well More
More