A c-reactive protein test measures the amount of c-reactive protein (CRP) in the blood to identify inflammation. There are many reasons doctors order c-reactive protein tests. High-sensitivity tests can evaluate the risk of coronary artery disease, while standard testing checks for infection and other conditions.
C-Reactive Protein Production
The body sends c-reactive protein into the bloodstream as a response to inflammation. Though inflammation is the body’s natural response to injury or infection, it also causes swelling, redness, and pain. C-reactive protein is primarily made in the liver but macrophages, lymphocytes, adipocytes, and smooth muscle cells also synthesize it.
Role of C-Reactive Protein
C-reactive protein is commonly used as a marker to evaluate infection and assess cardiovascular health, but it may be able to tell doctors much more. Current research indicates that it could also play a larger role in the immune response, including phagocytosis, cell death, and the production and release of cytokines, specifically interleukins, and tumor necrosis factors.
CRP at Baseline
Baseline c-reactive protein is determined by many factors, including blood pressure, lipid levels, age, weight, gender, and whether or not a person smokes. Genetic variations also play a role, and twin studies demonstrate that there is an inherited component to baseline c-reactive protein levels that is independent of age and weight. The results of normal c-reactive protein tests vary.
Hormone Replacement Therapy
Emerging research shows a significant increase in CRP in menopausal women who are undergoing oral hormone replacement therapy. Results from c-reactive protein tests nearly double in these women, indicating a significant increase in their risk of blood clots and cardiovascular disease. Interestingly, no increase in circulating CRP was found in women receiving hormone replacement therapy via a transdermal patch.
Elevated C-Reactive Protein
Elevated c-reactive protein tests are a strong predictor of many types of cardiovascular disease, including congestive heart failure, atrial fibrillation, and aortic valve disease, even in asymptomatic individuals. High-sensitivity tests can determine these risks. A CRP higher than 3 mg/L indicates an increased risk of coronary artery disease, and this risk is even higher when the person also has type 2 diabetes.
Unknown Role
C-reactive protein tests show increased levels during inflammatory diseases and infections, but the precise role of CRP in the development of these diseases is unknown. There are multiple forms of CRP, and evidence shows that some exhibit more pro-inflammatory properties than others. Targeted CRP therapies are of interest for treating some inflammatory conditions, but more research is needed.
Monitor Conditions
C-reactive protein tests are useful to identify new conditions, but they also monitor the progress of known conditions, including bacterial and fungal infections, inflammatory bowel disease, osteomyelitis, and some autoimmune diseases, such as rheumatoid arthritis and lupus. Doctors may use results from a CRP test to determine if these conditions are progressing or if current treatments are effective.
Symptoms
Doctors may order c-reactive protein tests when patients present with symptoms of a serious bacterial infection, such as fever, chills, rapid heart rate, nausea, vomiting, and rapid breathing. After treatment is initiated, a CRP test can evaluate whether or not it is working, as CRP levels should fall when the treatment is effective.
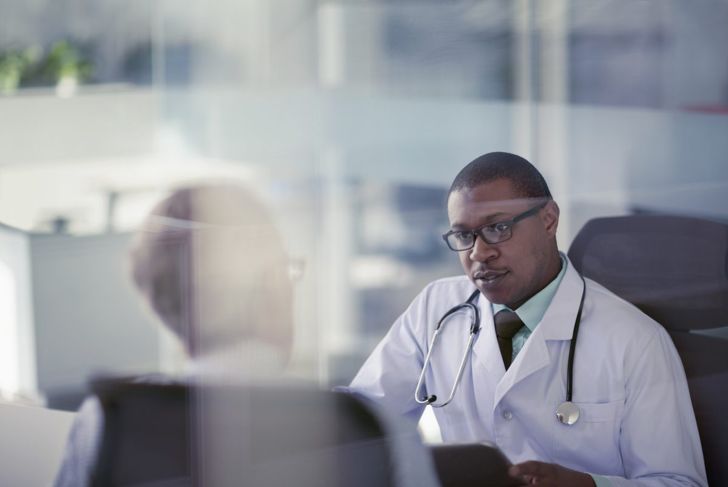
Risks of C-Reactive Protein Test
C-reactive protein tests are standard blood tests. A nurse or phlebotomist places a tourniquet around the arm and draws blood from a vein into a tube. The blood is then sent to a lab, and results are usually available within a few days. Risks are minimal and include bruising, fainting, feeling light-headed, and infection at the insertion site.
Results
Elevated results of c-reactive protein tests may indicate a few things. CPR greater than 10 mg/L indicates serious infection or chronic disease, and the patient will need additional testing to determine the cause. A slightly elevated result does not necessarily mean there is any underlying illness, however, smoking, being overweight, and a lack of exercise can elevate results.

 Home
Home Health
Health Diet & Nutrition
Diet & Nutrition Living Well
Living Well More
More