The thorax includes the lungs, heart, and thymus gland. Thoracentesis or pleural tap is a common procedure that physicians perform to either reduce the amount of fluid around the lungs or to analyze it. Doctors remove the fluid from the pleural space, the space between pleura — the tissue that covers the lungs — and the inside of the chest. Normally, the pleural space contains only a small amount of fluid, but some conditions lead to pleural effusion, a buildup of fluid around the lungs.
The History of Thoracentesis
In the fifth century B.C.E., Hippocrates first described a process he developed to drain the thoracic area. His Hippocratic texts instructed practitioners to remove fluids from the body using plant-based medications. If this process didn’t work, the texts told of a treatment where the physician cut the skin between the ribs and allowed any excess infected fluid to drain out. Once the fluid cleared, he inserted a hollow tube and completely drained the thoracic cavity. By the late 1950s, thoracentesis became a standard of care for draining fluid from the thoracic cavity. Since then, it has become a common and low-risk option. The materials doctors use to perform fluid removal have seen major advancements. There have also been significant strides in infection prevention, an issue that plagued the practice in its earliest forms.
Diagnostic and Therapeutic Thoracentesis
There are two types of thoracentesis.
- Diagnostic thoracentesis pinpoints the reason for the fluid buildup. Only about 20cc to 30cc of fluid is necessary to perform a lab analysis, to determine if there is an infection or another issue.
- Therapeutic thoracentesis usually requires the removal of a larger amount of fluid from the pleural space. Some conditions cause the cavity to quickly fill back up with fluid, so doctors leave the tube inside to enable continued drainage. Generally, they send a small amount of fluid for lab analysis.
Performing Thoracentesis
Thoracentesis is performed either on an outpatient basis or during a hospital stay, but the individual is usually awake. It requires sterile conditions. First, the medical team positions the patient in a sitting position or, in some cases, lying on their side. If sitting, the patient leans forward and rests their arms on supports positioned to open up the spaces between the ribs. Medical staff clean an area on the side, near the back, with antiseptic, then numb it with a local anesthetic. The physician inserts the needle between two ribs, into the chest cavity, and draws out the fluid.
Conditions That May Cause Fluid Buildup
The most common cause of fluid buildup in the lungs or lining of the lungs is congestive heart failure (CHF). Infection and pneumonia can also lead to pleural effusion. Physicians may diagnose cancers that have spread to the lungs, the lining of the lungs, or the chest wall after reviewing the lab results. Or, they may identify conditions such as lupus, pancreatitis, liver failure, kidney disease, or tuberculosis. Certain medications, chemotherapy, radiation therapy, and abdominal surgery can also lead to fluid buildup.
Complications of Thoracentesis
Few complications occur during thoracentesis, and if they do, they are minor. Some individuals complain of pain during the insertion of the needle, but the local anesthetic usually eases or prevents discomfort. Others report feeling faint during or after thoracentesis. Some may experience bleeding or minor bruising at the needle site. If the attending staff didn’t clean the area with antiseptic or failed to use a sterile technique, infection is possible. However, this is rare.
Risks of Thoracentesis
There are possible risks, but serious issues are rare.
- The physician may puncture a lung with the needle while retrieving a fluid sample. In most cases, the puncture heals very quickly. However, if it doesn’t, air builds up and causes the lung to collapse.
- Although it is extremely rare, there have been cases of liver or spleen punctures during thoracentesis. It is crucial that the individual remain still to prevent this complication.
- The patient could experience pulmonary edema, where fluid collects in the lung at the needle’s insertion site. This complication generally occurs only following the removal of large amounts of fluid.
Preparing for Thoracentesis
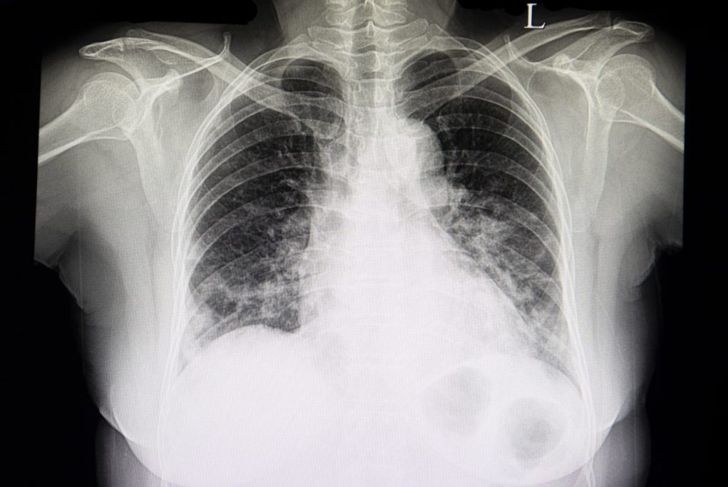
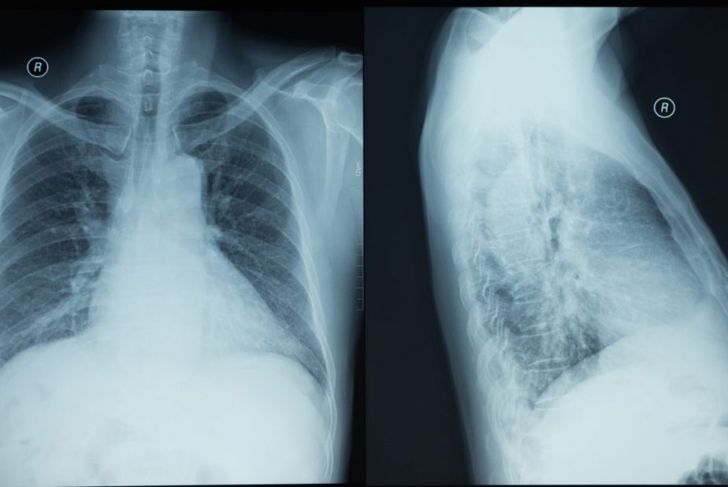
Many doctors perform an x-ray before starting thoracentesis, to pinpoint the exact location of the pleural effusion. Other physicians choose to perform an ultrasound as well as, or instead of, an x-ray. Individuals with conditions or who take medications that affect blood clotting should inform the physician beforehand. In some cases, the doctor may prescribe a sedative that causes the patient, most often a younger child, to feel sleepy during the procedure.
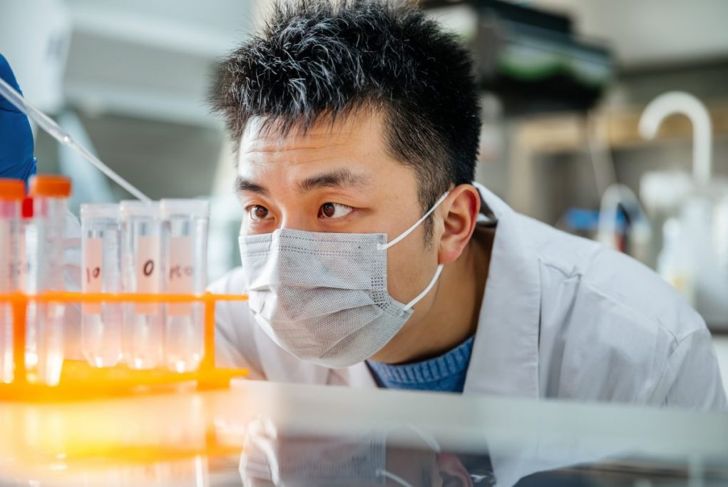
The Pleural Fluid Analysis
The lab’s testing should reveal the reasons for fluid accumulation. Transudate fluid (low protein and low specific gravity) indicates higher pressure in the veins and capillaries, which pushes the fluid out through the blood vessel walls and may lower the amount of protein in the blood serum. This usually indicates congestive heart failure or cirrhosis. If there is an injury or inflammation, the analysis will find the accumulated fluid is an exudate, meaning it is cloudy and high in protein or albumin. This indicates an infection such as pneumonia, tuberculosis, a bleeding disorder, or malignancy. It may also be a sign of autoimmune disease or exposure to asbestos.
Symptoms of Fluid Buildup
Several symptoms of fluid buildup may lead to the doctor ordering a thoracentesis. If the individual complains of painful or labored breathing or shortness of breath, has a fever, develops a dry cough, or has persistent hiccups, they could be experiencing pleural effusion. Some people find it difficult to breathe unless they are sitting up straight or standing erect.
After the Procedure
Thoracentesis usually takes about 15 minutes, depending on the amount of fluid. After removing the needle, the medical staff bandage the needle site. They then monitor the individual’s blood pressure and breathing to ensure the vitals are stable. Many doctors perform an x-ray after the procedure to catch potential complications. Some coughing afterward is normal but should stop within an hour. Discomfort or pain around the needle site and pressure in the chest are also normal side effects. Difficulty breathing, chest pain, increased pain or redness around the needle site, or a fever of more than 101 degrees require medical attention.

 Home
Home Health
Health Diet & Nutrition
Diet & Nutrition Living Well
Living Well More
More