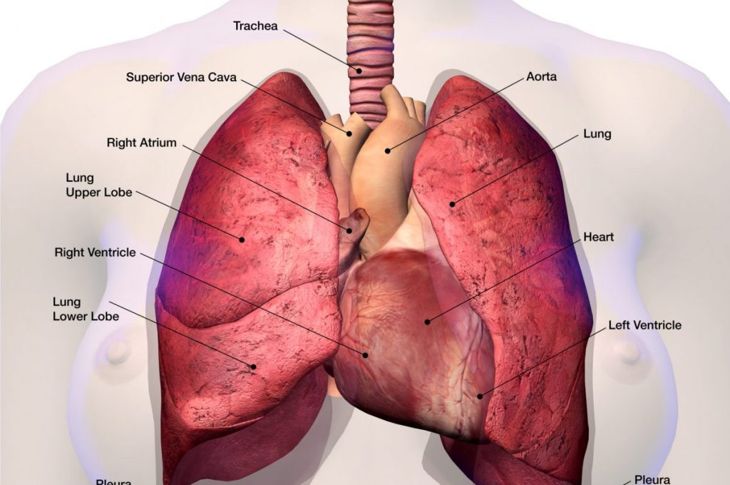
The superior vena cava (SVC) is a short, wide vein that moves blood from the head, neck, arms, and torso to the heart. It sits near the lymph nodes in the chest. Superior vena cava syndrome causes compression of the SVC and can eventually block blood flow to the heart. In most cases, this compression is gradual, but some illnesses lead to more rapid SVC compression. Doctors diagnose around 15,000 people with the condition each year. SVC syndrome is a medical emergency because it can be life-threatening. However, most people respond well to treatment.
Basic Facts About SVC Syndrome
The cardiovascular system depends on the SVC because it supplies blood to the heart. The thin-walled vein has no valves and is surrounded by rigid structures. As such, blood flowing through the vein creates very little pressure, making the vein more susceptible to compression or blockage. Both issues can lead to SVC syndrome. The condition can also lead to breathing issues due to swelling in the neck and upper body.
Causes: Malignancy and SVC Syndrome
Between 80 and 90% of individuals with SVC syndrome have some malignancy, such as malignant lung tumors or lymphoma. A tumor may grow into the SVC and cause a blockage or press against it and restrict blood flow. Sometimes, cancer causes a blood clot in the vein. Research shows that 50% of those individuals who contract SVC syndrome have non-small cell lung cancer, which causes the lymph nodes to increase in size. The enlarged lymph nodes squeeze the SVC and either slow blood flow or block it completely. Other types of cancer that may lead to the condition include
Squamous cell lung cancer
Adenocarcinoma of the lung
Non-Hodgkin lymphoma
Doctors have also diagnosed the condition in individuals with metastatic breast cancer, colon cancer, thyroid cancer, and immune system diseases such as Bechet’s syndrome, but these are rare instances.
Nonmalignant Causes of SVC Syndrome
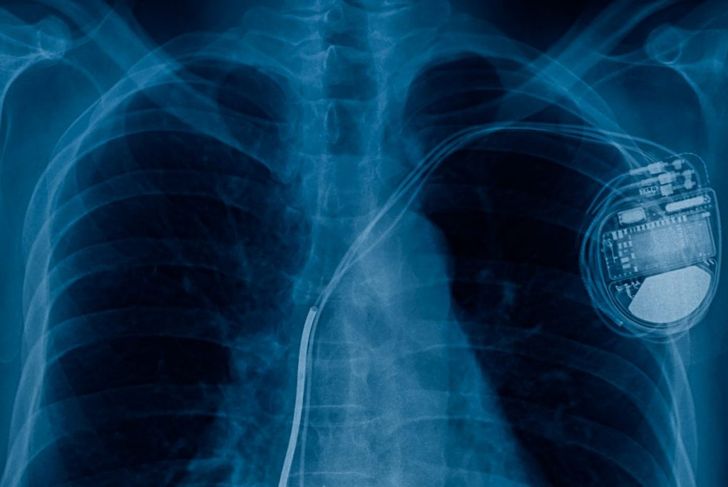
The remaining individuals with SVC syndrome also have vascular diseases such as aortic aneurysms, large vessel vasculitis, or, rarely, mediastinal fibrosis. Doctors have also discovered this syndrome in patients with tuberculosis, syphilis, lung infections, and actinomycosis, a rare bacterial infection that spreads through body tissues. A growing number of people with SVC syndrome first receive diagnoses of benign tumors such as teratoma, thymoma, or dermoid cysts. Researchers are also finding more and more cases in individuals with thrombosis resulting from pacemakers and central venous catheters. These devices can cause blood clots that interfere with blood flow.
SVC Syndrome in Children
Although rare, SVC syndrome may occur in children with cancer. Because a child’s trachea is narrower and softer than an adult’s, breathing can easily become restricted when there is swelling in the neck or upper torso. For this reason, once doctors diagnose the condition, they usually admit the child to ICU so medical staff can monitor vital signs, provide supplemental oxygen, and ensure adequate hydration.
Symptoms of SVC Syndrome
Signs of SVC syndrome develop slowly in most cases. Individuals usually notice swelling in their faces, necks, upper bodies, and arms. They may experience shortness of breath or find it difficult to breathe, which can lead to faster breathing. Sometimes, the skin takes on a bluish tint due to a lack of oxygen. Coughing is also a common symptom, and some people complain of headaches as well as nasal stuffiness. Rarely, do those with SVC syndrome experience additional symptoms, including
Hoarseness
Vocal cord paralysis
Chest pain
Difficulty swallowing
Fluid buildup in the arms
Pupil constriction, a sagging eyelid, and lack of sweat on one side of the face, also known as Horner’s syndrome
In more advanced stages, fluid builds up around the brain, which can cause dizziness and confusion.
Diagnosing SVC Syndrome
The first step toward diagnosis includes a thorough physical exam. Facial edema is often the most prevalent visual indication of the syndrome. Physicians perform a variety of diagnostic tests, including blood count and coagulation studies, to confirm or rule out SVC syndrome. They use a chest x-ray, MRI, CT scan, and ultrasound to identify the type and location of the blockage or compression. Physicians may apply a grading system based on the symptoms and their severity to establish a clear diagnostic and therapeutic plan.
Additional Testing
For those individuals with SVC syndrome resulting from malignancies, doctors often perform additional histologic testing to ensure an accurate diagnosis. The physician examines sample tissue and fluids from the body through minimally invasive techniques and may perform a biopsy of the lymph nodes above the clavicle if the ptient is not already diagnosed with a malignancy. They may also perform a bone marrow biopsy for patients they suspect have non-Hodgkin lymphoma or small cell lung cancer.
Treatment
The primary goals for treatment are to alleviate symptoms and treat cancer or underlying disease or infection. The treating physician considers patients experiencing central airway obstruction, swelling of the larynx, or coma resulting from cerebral edema as being in life-threatening states. Treatment includes securing the airway and providing breathing support, such as a ventilator, continuous positive airway pressure (CPAP) machine, or oxygen through a nasal cannula or mask based on the individual’s condition. Radiation therapy is a common treatment for those with SVC syndrome stemming from a malignancy.
Age and SVC Syndrome
More males than females develop lung cancer, so more men develop SVC due to malignant causes. Additionally, the majority of people who develop SVC syndrome caused by malignancy are between the ages of 40 and 60. Non-malignant or benign causes of SVC syndrome occur most frequently in people in their 30s. Researchers know of no link between benign causes of the syndrome and either sex.
Prognosis
Research suggests that without treatment, people with malignant SVC syndrome only survive for about 30 days. Survival rates are based on the underlying cause, not on the SVC itself; venous compression is usually not lethal. If the SVC syndrome is the result of a benign cause, there is no change in the survival rate. However, those who have SVC syndrome that is secondary to malignancy will have a survival rate based on its type. People with laryngeal or cerebral swelling experience a higher rate of life-threatening symptoms or sudden death.

 Home
Home Health
Health Diet & Nutrition
Diet & Nutrition Living Well
Living Well More
More