Physicians often prescribe calcium channel blockers to patients diagnosed with hypertension, especially those over 55 years of age, people of African or Caribbean descent, or people with diabetes. Calcium channel blockers can also treat circulatory conditions such as Raynaud’s disease. Medical professionals often choose them to treat chest pain or irregular heartbeat. Not only do these medications have modest side effects, but they are usually a safe option for pregnant and nursing mothers and older individuals.
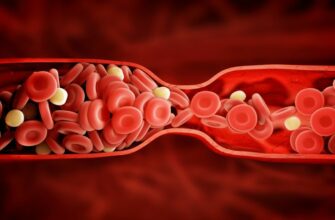
How Calcium Channel Blockers Work
Calcium is crucial for the regulation of heart-muscle functions and nerve transmission. It is an important element for the heart’s contraction mechanism, which supplies blood to the body. However, for some individuals, excessive calcium causes the heart to contract in a more robust manner, allowing higher levels of calcium to flow through the vessels, causing hypertension. Calcium channel blockers or CCBs slow the rate at which calcium passes into the heart muscle and the blood vessel walls. As a result, the vessels relax and allow the blood to flow more easily. There is less demand for oxygen from the heart, which thus lowers blood pressure.
Types of Calcium Channel Blockers
Pharmacologists sometimes refer to calcium channel blockers as calcium antagonists. They divide CCBs into three classes: dihydropyridines, benzothiazepines, and phenylalkylamines.
Dihydropyridines are L-type calcium channel blockers. Doctors prescribe them to reduce vascular resistance and arterial pressure, which makes them an effective treatment for hypertension. Dihydropyridines may cause tachycardia or rapid heart rate in patients with angina.
Benzothiazepines work on both the arteries and the heart muscle. They effectively reduce arterial pressure but produce a lower level of cardiac stimulation than dihydropyridines.
Physicians prescribe phenylalkylamines to treat angina because they cause less tachycardia. This type of CCB reduces the amount of oxygen the heart muscle needs. Additionally, phenylalkylamines reverse coronary vasospasm, which causes constriction of the coronary artery and stroke-like symptoms.
Effectiveness in Patients of African Caribbean and South Asian Descent
Hypertension is the primary cause of cardiovascular disease and death globally, according to the World Health Organization. Some ethnic groups tend to develop hypertension at an earlier age. Research indicates that those of African, Caribbean, and South Asian ancestry receive hypertension diagnoses in higher numbers. People with Caribbean ancestry have a higher prevalence of hypertension than black West African or Caucasian individuals. Despite having lower cholesterol levels than Caucasians, South Asian people exhibit more severe atherosclerosis and ischaemic-end organ damage due to hypertension. Researchers say that African Caribbean patients respond better to CCBs and diuretics than to other types of pharmacological treatments such as ACE inhibitors. Studies also suggest that South Asian individuals do not receive the same benefit from CCBs. Research is ongoing to determine the effectiveness of specific antihypertensive agents for various ethnicities.
CCBs and Older Patients
As people age, so too does their physiology. Hypertension in patients 65 years of age and older is not only more prevalent, but it is also more difficult to control. Studies show CCBs are highly effective in preventing strokes in older patients, primarily attributed to their ability to lower blood pressure without major side effects. Although diuretics are less expensive, health professionals have voiced concern that even moderate doses may increase the development of type 2 diabetes, insulin resistance, and hyperkalemia in older patients.
Side Effects of CCBs
Most people who take CCBs report no side effects. Physicians attribute some symptoms to the body adjusting to new medication or an increase in the dosage of the CCB. Swollen ankles are the most common complaint. In rare cases, people experience drowsiness, headaches, nausea, dizziness, or constipation. Some individuals report skin rashes or a flushed face. Some men say they feel the need to urinate more during the evening hours. In rare cases, patients complain about swollen or bleeding gums after starting the medication. Patients should notify their physician of any side effects.
Other Types of Hypertension Medications
Physicians prescribe a wide variety, and sometimes multiple types, of medications to treat hypertension.
Diuretics help eliminate sodium and water from the body, which allows the heart to pump less blood and lowers blood pressure. However, doctors avoid prescribing them to people with gout or diabetes.
ACE inhibitors lower blood pressure and prevent the kidneys from retaining fluid and sodium. Doctors do not recommend ACE inhibitors for those with poor kidney function due to possible potassium retention. Pregnant women or those who plan to become pregnant should avoid ACE inhibitors as studies link them with fetal abnormalities.
Beta-blockers reduce the heart’s oxygen consumption, which lowers heart rate and blood pressure. Doctors also prescribe beta-blockers for angina and hypertension.
A physician often prescribes CCBs along with other types of blood pressure medications or with a medication that lowers cholesterol.
Magnesium: A Natural CCB
According to animal studies and current research, magnesium is a natural calcium channel blocker. Physicians may suggest an increase in dietary magnesium for younger people with elevated blood pressure not yet advanced to hypertension. Brown rice, cashews, oat bran, bananas, avocados, spinach, black beans, and soy are rich sources of magnesium. However, for people already taking CCBs, it is important to talk to a physician before increasing the intake of magnesium-rich foods.
CCBs During Pregnancy
If a pregnant or lactating woman experiences hypertension, the doctor may prescribe CCBs. Both obstetric and pediatric specialists say the risks are minimal and the medication does not harm the mother or the child. According to the American Academy of Pediatrics, small amounts of CCBs may pass into the breast milk but will not harm the infant. Due to a possibility of hypotension, however, the AAP also states that medical attendants should monitor the infant’s blood pressure. Physicians may also prescribe CCBs to women experiencing preterm labor before 37 weeks. CCBs relax uterine contractions, which can postpone a preterm birth.
Treatment for Hypertension With CCBs
In the past, doctors would not prescribe medications for hypertension unless the patient’s blood pressure reached 160/100. However, numerous studies and research findings indicate doctors should consider medication for stage 1 hypertension, which is 130/90 to 139/89, to prevent further increases in blood pressure. The National Institute for Health and Clinical Excellence advises a once-per-day dosage of CCBs and suggests physicians prescribe generics when possible. Pharmacology experts suggest starting patients at the lowest possible dose and increasing it until blood pressure is under control. In some cases, such as stage 2 hypertension or blood pressure of 140/90 or higher, the physician may prescribe a combination of two drugs.
Medications and Foods to Avoid When Taking CCBs
Some medications may increase or decrease the effectiveness of CCBs, so it is crucial the doctor be aware of any medications their patient is taking when they prescribe calcium channel blockers. Potentially problematic medications include beta-blockers, ACE inhibitors, antiarrhythmics, diuretics, digitalis, and some eye medications. Azole antifungal agents, such as the medication used to treat athlete’s foot, can increase the level of CCBs and cause adverse effects. Studies show that grapefruit juice prevents the body’s ability to absorb CCBs. Individuals should wait a minimum of four hours after taking the medication before consuming grapefruit or drinking grapefruit juice. Additionally, doctors advise patients taking CCBs to avoid smoking, as the combination is more likely to cause tachycardia.

 Home
Home Health
Health Diet & Nutrition
Diet & Nutrition Living Well
Living Well More
More