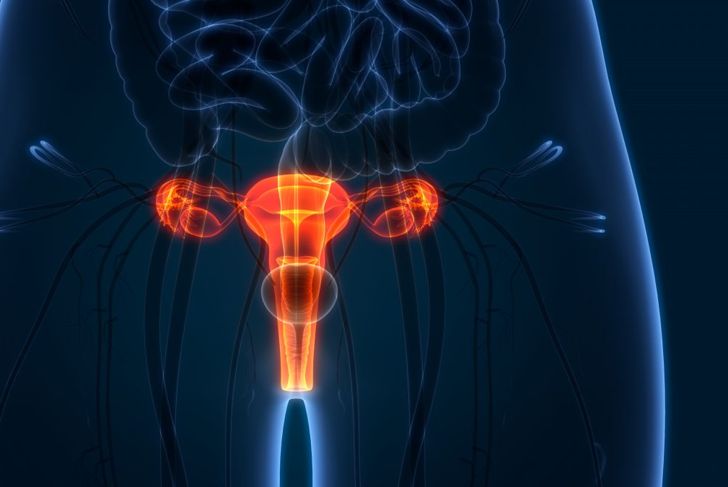
Medical issues affecting the uterus, hormone imbalances, and other conditions can cause menorrhagia, prolonged or abnormally heavy bleeding during a woman’s period. While most treatments revolve around addressing the underlying problem, medications and surgical procedures can relieve the secondary condition. Many women accept difficult periods as typical, but it is important to recognize signs that could point to medical concerns.
Causes of Heavy Periods
Many issues can cause menorrhagia. In the uterus, growths such as uterine polyps or fibroids can result in the condition. Hormonal imbalances can delay ovulation and lead to a thickened uterine lining, causing heavy bleeding and clotting during periods. Blood disorders like von Willebrand Disease or other platelet function disorders, as well as some medications [https] can also lead to menorrhagia.
Signs of Menorrhagia
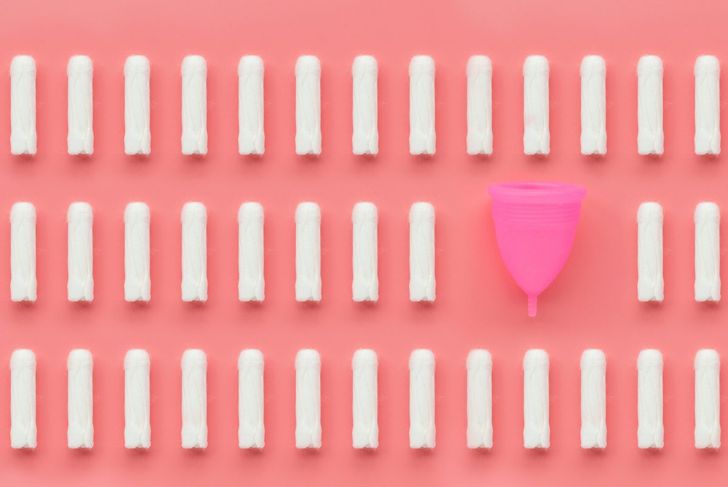
Heavy menstrual bleeding longer than seven days may be an indication of menorrhagia. A person with menorrhagia may also have a flow that soaks through one or more sanitary products several hours in a row, and may need to change pads or tampons during the night. A person with menorrhagia may be unable to participate in regular daily activities and often experiences lower back and abdominal pain during periods.
Are You At Risk?
A woman’s risk of developing menorrhagia varies by age and underlying medical conditions. Adolescent girls are at risk of having menorrhagia due to anovulatory, or eggless, menstrual cycles, which may also occur more often as a woman reaches menopause. Without egg release, the hormone progesterone is low, causing heavy menstrual bleeding. Mature women with uterine pathologies, such as fibroids, polyps, and cancer, also face an increased risk of menorrhagia.
Complications of Menorrhagia
Left untreated, menorrhagia can lead to serious complications. Excessive blood loss can cause anemia, reducing oxygen delivery and weakening the body. Menorrhagia can also lead to iron deficiency anemia as the body uses up iron to make hemoglobin. Both kinds of anemia cause pale skin, weakness, and fatigue. Menorrhagia can cause dysmenorrhea or painful menstrual cramps. These complications can become serious and require hospitalization.
How Menorrhagia Is Diagnosed
A healthcare provider will ask about a patient’s medical history and menstrual cycles to diagnose menorrhagia. When a tampon or pad must be changed more frequently than every two hours or when clots are larger than a quarter, the physician is likely to diagnose menorrhagia. After a diagnosis, the doctor can run blood tests to identify iron deficiency, anemia, or other clotting disorders. A Pap smear tests for inflammation or cancer in the cervical cells. Ultrasound images the genitourinary system to look for growths or masses.
Treatment with Medication
Medicinal therapies can treat menorrhagia. Oral contraceptives regulate the period and prevent prolonged or acyclical bleeding. A component of hormonal birth control, progesterone, can regulate menstrual blood loss. Nonsteroidal anti-inflammatory drugs (NSAIDs) treat the pain associated with menorrhagia, with the added benefit of reducing menstrual blood flow. Iron supplements can help regulate low iron caused by iron deficiency anemia.
Peter Dazeley / Getty Images
Procedures for Treatment
Some women require surgery to treat their menorrhagia. Operations to treat uterine fibroids include myomectomy, endometrial ablation, uterine artery embolization, and focused ultrasound surgery. These strategies remove the fibroids, cut off their blood supply, and prevent their regrowth. Alternatively, a radical hysterectomy can remove the entire uterus and cervix, stopping menstruation entirely.
Who Is Affected
Menorrhagia is one of the most common problems reported to doctors in the United States, affecting tens of millions of people each year, an estimated one in five women. It can occur in people of every demographic, regardless of background. Underlying conditions can cause menorrhagia even in postmenopausal women.
Managing Menorrhagia
People with menorrhagia find various ways to manage their condition. Over-the-counter medications like ibuprofen can reduce menstrual bleeding and pain, but taking them long-term is not ideal and can lead to other issues. A hot water bottle can alleviate cramping and back pain. Unfortunately, some women must limit physical activity on days when they are bleeding excessively, due to anemia and weakness. Others plan their days around proximity to a bathroom and sanitary products and feel they must wear dark clothing to ease the anxiety of staining.
When To Seek Help
Though discomfort and heavy menstruation have at-home remedies, it is important to know when to contact a healthcare provider. Any woman who experiences bleeding between periods should discuss the issue with her doctor. If heavy bleeding soaks through one sanitary product an hour for more than two hours, or if there are large, thick clots, it is also imperative to speak to a physician. Any bleeding at all after menopause is cause for concern and immediate medical evaluation.

 Home
Home Health
Health Diet & Nutrition
Diet & Nutrition Living Well
Living Well More
More