Hypovolemic shock is a sudden, severe drop in the body’s total fluid volume. This type of shock happens in four stages. Multiple organ failure occurs because the heart cannot pump a sufficient amount of blood and other fluids through the body. Children and older adults have the highest risk of developing this life-threatening condition, but it can affect people of any age. Recognizing hypovolemic shock quickly and getting emergency medical treatment is essential to avoiding long-term damage or death.
Effects of Hypovolemic Shock
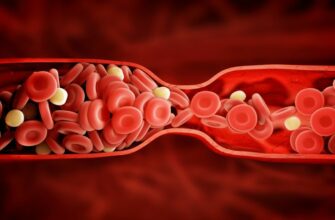
The circulatory system contains blood and fluids that carry oxygen, nutrients, and other components to tissues and organs. Blood also carries waste products to that get broken down or excreted from the body. The exchange of oxygen and carbon dioxide in the lungs depends on the circulating fluids pumped by the heart. When circulating blood volume is too low to maintain circulation, blood pressure drops rapidly and organs begin shutting down. Brain damage is possible after only two minutes without oxygen, so it is vital to treat hypovolemic shock immediately.
Risk of Dehydration
The best time to drink fluids is before dehydration occurs. People lose water and electrolytes during illness through fever, vomiting, and diarrhea. Exercise, hot and humid weather, or physical labor prompt sweating. Injuries leading to blood loss are unexpected and unpredictable, but most can still avoid dehydration and electrolyte imbalances. Make sure to drink extra fluids during illness, strenuous activity, or hot weather.
Risk of Blood Loss
Severe wounds or injuries sustained in accidents are obvious sources of blood loss. External injuries are visible but blunt force trauma can also cause hidden internal injuries. Blood loss with no external cause often stems from internal bleeding in abdominal organs or ulcers in the digestive tract. Less common causes of internal bleeding include ruptured ectopic pregnancies, endometriosis, and other types of vaginal bleeding.
Early Symptoms
Early symptoms of hypovolemic shock include nausea, vomiting, dizziness, fatigue, headache, and sweating. Initial symptoms are hard to recognize in the absence of an external wound or accident because many common illnesses and other factors can cause them, as well.
Advanced Symptoms
Advanced symptoms include clammy and pale skin, confusion, weakness, and feeling dizzy or light-headed. Rapid and shallow breathing, a rapid heart rate with a weak pulse, and decreased urine output often occur. The final symptoms are blue lips and fingernails, due to a lack of oxygen, followed quickly by a loss of consciousness. Death is almost certain without medical intervention before, or in response to, these later symptoms.
Stages One and Two
Stage one of hypovolemic shock may not include any symptoms or only very mild ones. Initially, the affected person’s blood pressure may be stable, and breathing is likely normal. The most noticeable symptom is paleness. During stage two, blood pressure is still in a normal range but diastolic pressure may rise. Anxiety, sweating, and general restlessness are the most apparent symptoms. The first two stages of hypovolemic shock can progress very quickly or slowly, depending on the cause.
Stages Three and Four
Stage three of hypovolemic shock progresses rapidly. By this point, the body has lost over a third of its total blood volume. Blood pressure and heart rate spike. Breathing also becomes difficult, quick and shallow. Symptoms manifest as extreme anxiety and agitation, combined with pale, cold, and sweaty skin. These symptoms continue to intensify as the individual reaches stage four. The most advanced symptoms at this point is the loss of consciousness.
Diagnosis
Doctors diagnose hypovolemic shock through observation and testing. The doctor measures respiration, heartbeat, blood pressure and body temperature. Blood tests identify electrolyte imbalances, measure liver and kidney function, and help determine the extent of blood loss. They also measure clotting factors and red blood cell count in case a transfusion is necessary.
Treatment
Treatment of hypovolemic shock varies depending on the cause. Initial treatment is always focused on stopping fluid loss and stabilizing blood volume with intravenous fluid. Plasma transfusions can replace lost red blood cells. Severe cases may require platelet replacement if the blood is too diluted to clot. Once the patient stabilizes, the medical team will treat the underlying injury or illness.
Prognosis
The prognosis varies depending on the stage of hypovolemic shock. It also depends on the rate of blood loss and the amount of total blood volume lost. Organs may be permanently damaged, especially the kidneys and brain. Complications are more severe when the individual has heart disease or on blood thinners. Prior heart attack or kidney disease and advanced age also worsen complications. Recognizing symptoms and accessing treatment quickly provides the best chance for a full recovery.

 Home
Home Health
Health Diet & Nutrition
Diet & Nutrition Living Well
Living Well More
More